Photo by Susan Wilkinson on Unsplash
What is trauma?
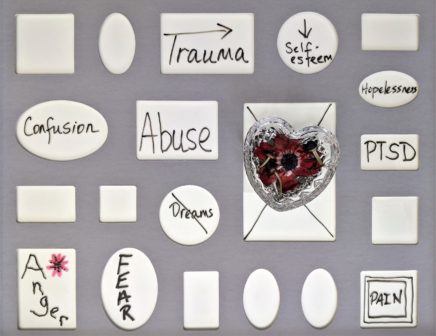
Trauma refers to the emotional response experienced following exposure to a distressing life event or situation. It can result from direct or indirect exposure, i.e., we have experienced the situation first hand, witnessed it, or heard that the event occurred to someone we know. Traumatic experiences may include a serious accident, physical or sexual assault (actual or threatened), sudden violent death, natural disaster, and war.
Common responses to trauma
When we are exposed to a threatening situation, it infringes on our sense of safety and security, leading to a level of psychological distress and belief that our environment is no longer safe. Emotional responses can vary from person to person, but typically include feelings of fear, anxiety, helplessness, hopelessness and impacts to self-esteem.
Posttraumatic stress disorder
Psychological distress is a common experience following exposure to a traumatic event however for some individuals the impact of trauma can be long lasting and lead to the development of a trauma-related disorder, such as posttraumatic stress disorder (PTSD). Symptoms of PTSD include:
- Recurring distressing memories and dreams of the event
- Feeling as though the distressing event was happening again (flashbacks)
- Avoidance of situations that remind you of the event
- Difficulty remembering important aspects of the event
- Negative beliefs about self and others
- Persistent fear, anxiety, guilt or anger
- Feeling detached from others
- Loss of interest in enjoyable activities
- Feeling hypervigilant and easily startled
- Reduced concentration
- Impacts to sleep patterns
Please note, this is not an exhaustive list of symptoms, but provides a snapshot of some of the impacts of PTSD. Diagnosis is based on many factors and not solely on experiencing the above symptoms.
Does exposure to trauma result in PTSD?
The experience of trauma may lead to the development of PTSD however, this is not always the case. Development of a trauma-related disorder, such as PTSD, is influenced by more than just exposure to a traumatic event. As individuals, we all have different ways of coping, which is related to our personality and past personal experiences. Often, exposure to trauma can severely rattle our perception of self and can impact on our sense of self-worth and self-esteem. Other factors to consider include the nature and severity of the event. In addition, the way in which the incident is interpreted and understood immediately following the trauma, and the way in which we store the incident in our memory, can play an integral role.
How trauma memories are stored
The hippocampus is the part of the brain that stores memories. It encodes memories and takes a bird’s-eye view of a situation, which incorporates a lot of detail. When you remember something, you don’t recall it exactly the way it was encoded. Every time you remember something, you are re-creating it every single time. Your hippocampus time stamps the memory with when it happened and how long it lasted. And as you move further into the future, the memory becomes more distant. This relates to a good/pleasant memory.
When you are in a threatening situation, the way in which memories are encoded and stored becomes impacted. When faced with a traumatic event, you are under enormous stress and your cortisol levels increase, which means that the hippocampus cannot function in the same way it does when you are not stressed. The hippocampus is covered in cortisol receptors and when you are stressed, the cortisol floods into the hippocampus. This means that the hippocampus is not fully activated when you are encoding this memory. You are therefore encoding things differently to what you would otherwise. It changes how you remember things and how you recall them later. In stressful situations, the hippocampus does not take a bird’s-eye view of the situation, rather, it takes smaller close-up detailed pictures, almost like ‘zooming in’ on a camera lens. This happens because the brain starts to focus on pieces of information it perceives as important, in that situation. Therefore, the information that gets encoded is the close-up pieces. Another thing to note is that when faced with a traumatic situation, the hippocampus may fail to put a time stamp which tells you how long something lasted. The memory may seem out of order and all over the place because of the way it was encoded. If your hippocampus didn’t time stamp, then instead of remembering things you re-experience them, and therefore every time you think of that situation, you feel as though it is happening again. Thus, trauma memories do not age appropriately.
Treatment
Psychological therapy can help to manage symptoms following exposure to trauma. This includes, but is not limited to, building emotion regulation skills, relaxation strategies, shifting negative beliefs, increasing self-esteem, and reprocessing trauma memories.
If you are seeking support following exposure to a traumatic incident, our team of psychologists are here to help. Feel free to give our clinic a call on 9802 4654 and our friendly admin team can assist by recommending the best practitioner for your care.
References
Kessler, R. C. (1995). Posttraumatic Stress Disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048.
Nijdam, M. J., & Wittmann, L. (2015). Psychological and Social Theories of PTSD. Evidence Based Treatments for Trauma-Related Psychological Disorders, 41– 61. doi:10.1007/978-3-319-07109-1_3
Sweeton, J. EMDR skills for trauma. Training workshop (completed Nov 2021).
Yehuda, R. (2004). Risk and resilience in posttraumatic stress disorder. Journal of Clinical Psychiatry, 65, 29-36.