The Craving Cycle: A CBT Concept for Managing Addiction
laura on 16/06/2023

Photo by Külli Kittus on Unsplash
In psychological therapy, we’re almost always looking to make progress. This often comes back to behaviour change – i.e., how we’ll behave differently in the face of difficult situations and feelings. In therapy targeting addiction, our behavioural goal is basic but difficult – we want to cease the addictive behaviour causing us harm.
If you’re someone who struggles with addiction, Cognitive Behavioural Therapy (CBT) is one of a host of different treatments that can help you recover. CBT aims to a) provide education about the various thoughts, feelings, and behaviours that maintain addiction, b) devise tailored strategies for encountering addiction-related thoughts and feelings, and c) making meaningful changes to behaviour to reduce or cease the cycle of addiction.
This blog will be talking about The Craving Cycle – one of the most fundamental concepts in CBT for addiction. As it applies to a whole range of different addictions – including drugs, alcohol, gambling and food – we’ll refer to all of things generically as the ‘addictive object’.
What is craving?
Craving is the physiological and psychological response to our addiction-related triggers. Triggers can be external (e.g., people, places, things, situations) or internal (e.g., thoughts, memories, images, feelings).
In CBT, we consider a craving any response that increases your motivation to engage in addictive behaviour. It could be an overwhelming sense of stress, intolerable anxiety, or just an irresistible pull towards whatever we’re craving. Understandably, we become motivated to ‘dampen’ these feelings by using the addictive object.
For better or worse, our choice to engage in the addictive object has consequences. The Craving Cycle is called a ‘Cycle’ for a reason – the more we use an addictive object to dampen our cravings, the more frequent and intense our cravings will become in response to our triggers. If we pull into the McDonald’s drive-thru every night after work, we’re only going to become more and more stimulated when we see those golden arches!
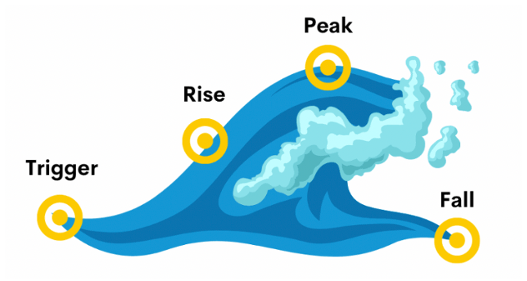
We often think of craving as a ‘wave’ – and on a graph of time vs. intensity, it literally looks like one.
Image source: https://www.greatergeelongpsychologyclinic.com.au/blogs/surfing-your-way-to-new-habits
The fact a craving looks like a wave – i.e., reaches its intensity slowly and then dissipates quickly – leads us to call a key CBT strategy ‘urge surfing’. In urge surfing, we are up-skilling ourselves in the ability to handle difficult craving-related feelings.
What is the Craving Cycle?
The Craving Cycle is understood as having four component parts – 1) the trigger, 2) the addiction-related thought/s (i.e., thoughts that justify using the addictive object), 3) the craving itself, and 4) the choice to use.
Trigger Thought/s Craving Choice to Use
How can I better manage these cravings?
The first and most basic step is to, as much as possible, eliminate both a) triggers, and b) access to the addictive stimulus. Eliminating triggers can be easy in some cases (e.g., not driving past an outlet for the object) but harder for others (e.g., inevitable thoughts, memories, and feelings). This is why eliminating access is so critical – if we have access to the addictive object in our household, we’re vulnerable to lapsing if/when a craving arises.
When most people think about eliminating triggers and/or access, they can become pretty overwhelmed. Sometimes, it’s near-impossible to totally eliminate triggers or access. In those cases, it becomes critical to learn how to ‘urge surf’ and deal with the difficult thoughts and feelings associated with this. Once we have a tried-and-true strategy to manage these, the urge to use becomes less daunting. In CBT, urge surfing is one of the most important strategies you’ll learn.
The good news is that the more we crave without using the addictive object, the less intense and frequent our cravings become. Cravings are a ‘use it or lose it’ response – the less we give in to them, the less likely they are to return. For this progress to be consistent, though, our behaviour also needs to be consistent. Lapses and relapses, no matter how short, can bring our cravings roaring back.
If you’re looking for some individualised and structured support, and want to start beating your cravings, the team at Your Mind Matters can help. Give us a call to book in an initial consult, and make mention if addiction is a particular concern for you.
There are also support groups available in the community (such as SMART Recovery and various Twelve Step programs) that can make recovery a less lonely experience. Lots of self-help resources can be found online, and online/telephone support services are listed below:
Alcohol and Drug Counselling Online: https://www.counsellingonline.org.au/
Positive Choices (Drug and Alcohol Information): https://positivechoices.org.au/
Family Drug Support: 1300 368 186
Gambling Help Line: 1800 858 858
Lived Experience Telephone Support Service (LETSS): 1800 013 755
References
Centre for Addiction and Mental Health. (2020). Cognitive behavioural therapy (CBT) for problem gambling. Centre for Addiction and Mental Health. https://kmb.camh.ca/ggtu/knowledge-translation/cognitive-behavioural-therapy
Fong, T. W. (2006). Understanding and managing compulsive sexual behaviours. Psychiatry (Edgmont), 3(11), 51-58.
Gonzales, M. (2020, February 27). What is Cognitive Behavioral Therapy (CBT)? DrugRehab. https://www.drugrehab.com/treatment/types-of-therapy/cognitive-behavioral-therapy/
McHugh, R. K. (2010). Cognitive-Behavioral Therapy for Substance Use Disorders. Psychiatry Clinics of North America, 33(3), 511-525.
Naqvi, N. H. (2015). Cognitive regulation of craving in alcohol dependent and social drinkers. Alcohol: Clinical and Experimental Research, 39(2), 343-349.
National Institute of Clinical Excellence. (2011, February 23). Alcohol-use disorders: Diagnosis, assessment and management of harmful drinking (high-risk drinking) and alcohol dependence. National Institute of Clinical Excellence. https://www.nice.org.uk/guidance/cg115
This blog was written by Patrick (Paddy) Carey – Clinical Psychologist at YMM.
Paddy works with adults presenting with anxiety disorders, mood disorders, trauma and stressor-related disorders, obsessive-compulsive disorders, substance and gambling issues, psychosis spectrum disorders, and grief and loss. He is trained in Cognitive Behaviour Therapy (CBT), Acceptance and Commitment Therapy (ACT), Cognitive Processing Therapy (CPT), Metacognitive Training (MCT), and mindfulness approaches.
Paddy is focused on developing warm, trusting, and strengths-based relationships with clients. He recognises that his clients are the foremost experts in the room, and unearthing their own expertise is crucial to applying his skills. Most importantly, he’s invested in moving towards a client’s own definition of recovery – i.e., what will be the most meaningful and fulfilling life for them beyond their current struggles.
To learn more about Paddy, check out the “Our Team” page on our website! https://yourmindmatters.net.au/our-team/
- Category: Addiction